Did you know that advance care planning inspires your patients and reduces your risk for burnout?
Take the CAREPROVIDER QuizDoes this fit you? Are You ...

- avoiding advance care planning conversations due to lack of training, time or incentives?
- frustrated that your patients’ DNR/DNI conversations are not with you, who they know and trust, but with "strangers" – emergency room doctors, hospitalists, intensivists?
- frustrated by your patients’ initial unwillingness to talk about advance care planning?
- second-guessing your own judgment because you lack opportunities to explore what your patients really want?
- frustrated by patients who want “everything done” not realizing this may cause more harm than good?

- losing - or have already lost - your passion for taking care of your patients?
- talking AT your patients rather collaborating with them - a must when managing chronic diseases?
- seeking ways to reduce unnecessary emergency visits and hospital inpatient days?
- looking for ways to help your patients be better decision makers and more engaged in their care?
For DOCTORS: CaringEnd Empowerment Path
Do you avoid advance care planning conversations for lack of training, time, or incentives?
Are you burning out because you’re held responsible for patient decisions over which you have no control?
Are you frustrated by practice demands that hamper your ability to connect with your patients?
You can regain your passion, curiosity, and mastery!
Shift your mindset, shift your patient’s mindset: create advance care planning conversations that fit your workflow, and build trust and gratification with CaringEnd Empowerment Path.
CaringEnd Empowerment Path is a system based on the CARES modular system I created which describes your patient’s medical life journey as a road trip with mileposts. This system help you partner with your patient and with their family caregiver.
CARES stands for Category, Awareness, Rating, Expectation and Self-management.
CARES forms the components of a medical life journey roadmap. This roadmap concept is your tool for shared decision-making. It supports you in the challenging task of organizing and presenting information to your patient and their family caregiver while acknowledging your limited time and resources. It helps them make confident decisions and builds their trust.
Category: a framework for repurposing your Problem List in a novel way that reignites your curiosity and sets the foundation for your advance care planning. Awareness: a framework for gaining meaningful emotional, social, and spiritual inputs that engage your empathy. Empathy is your active approach for exploring your patient’s medical life journey through their eyes which helps you be more realistic in your assessment and planning. This builds the buy-in and trust that makes your care plan more likely to succeed. This approach creates opportunities for vital feedback when the disease course becomes complicated. The result is less unwanted care, particularly at the advanced stages of life and chronic disease where quality of life benefits more than length of life. Rating: a framework for interpreting where your patient is on their medical life journey, and a context for discussing prognosis. Expectation: a framework for interpreting and discussing prognosis. Self-management: a platform for shared decision making through the novel use of chronic disease action plans.
WHO IS IT FOR:
The Caring End C.A.R.E.S. system is mainly for primary care doctors and geriatricians, nurse practitioners and physicians’ assistants licensed to create treatment plans, write orders, and prescribe. Clinician educators and palliative/hospice professionals can also benefit. Professionals such as social workers and case managers, life and wellness coaches, financial planners who want to add a medical readiness aspect to their estate planning offerings, and caregivers and other interested laypersons may find it useful as well.
BENEFITS:
Caring End C.A.R.E.S. System as expressed in the CaringEnd Empowerment Path adapts to your unique personality and workflow, much as your history and physical adapts to your workflow and the needs of the situation. It creates opportunities for you to view your patient and their clinical challenges with fresh eyes. It provides you with tools to engage your patient and family caregiver in shared care planning for the present and for the end of life. Rather than be frustrated by being blamed for patient decisions over which you have no control, you can prepare your patients and family caregivers to choose less unwanted and unnecessary care that meets their needs.
WEBSITE:
www.CaringEnd.com
www.CareProviderQuiz.com
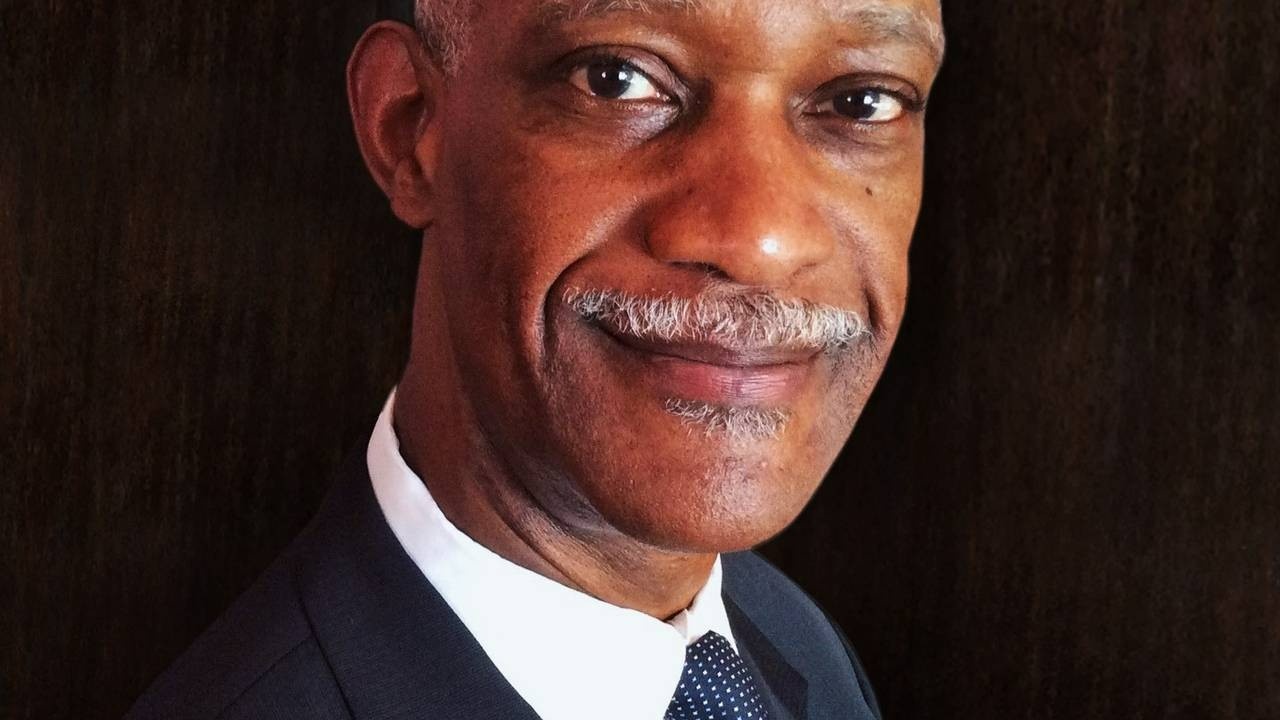
NICE TO MEET YOU
I am Forrest Jones MD
Forrest Jones MD, FAAFP, has been a Family Physician for over 40 years. He earned his doctorate in medicine at the Northwestern Feinberg School of Medicine and completed his Family Medicine residency at Cook county Hospital in Chicago.
When he become his parents’ medical power of attorney, he realized he wasn’t having end-of-life talks with his patients: too many barriers.
While searching for a solution, he discovered that conversations with his patients around advance care planning revived his passion by feeding his curiosity and empathy. This built his patients' trust, and reduced his risk for burnout.
He enjoys free time with his wife Roberta, children and grandchildren. He also delights in good food, travel and music.
One of the toughest most sacred callings that we have is to care for our patients at the end of their life.
I can help you approach advance care planning conversations like you approach your H & P.
I want you not just to survive, but to thrive.
By the end of this program, you will:
- Have a system and process that reduces your risk for burnout by reviving your clinical curiosity and your empathy.
- Confidently initiate elements of end-of-life conversations in a way that fits your style of practice.
- Recognize the difference between a crisis "delivering bad news" conversation and a proactive advance care planning conversation.
- Have a system and process that improves your patient satisfaction scores and can reduce unnecessary emergency visits and inpatient admissions.
- Use your patient's advance care plan for patient skill-building and decision making. This encourages patient responsibility and engagement in their care plan.
- Use your patient's advance care plan not just to prepare your patient for a "good dying" in the future, but to promote their wellbeing in the present.
How I came to start this journey ...
Some time ago, I was caring for a 94-year-old gentleman. An active senior, he lived alone in his small home, doing most everything for himself. Basic self-care tasks like eating, bathing, grooming, and getting dressed, were not obstacles. He didn’t shop for himself or do housekeeping, but he managed his money, medications, and cooking.
One day I made a visit with the goal of documenting his advance care plan. So, I asked him, “If your heart should suddenly stop beating, would you want everything done; would you want CPR (cardiopulmonary resuscitation)?”
After a thoughtful moment, he replied: “It depends.”
His answer surprised and frustrated me. It was not the simple “yes” or “no” I had naively expected. Yet it was most reasonable. I should have known better. My other patients probably have the same answer in mind, though I never heard them use those words. In fact, it is the reply I myself would give if asked.
This gentleman’s wise answer, “It depends,” started me wrestling with my own question: “Depends on what?”
There is no one-size-fits-all answer to this question. It is a personal one and varies from individual to individual. Even in the same individual, one’s answer to “Depends on what?" and “When is enough enough?” evolves as age and health
My struggle with this question birthed an idea for the project I now call Caring End.